Trump Administration Blocks Medicare From Covering Obesity Drugs — Why It Matters
The Trump administration has decided not to go forward with a proposal for Medicare and Medicaid to cover high-demand obesity treatments.

Profit and prosper with the best of Kiplinger's advice on investing, taxes, retirement, personal finance and much more. Delivered daily. Enter your email in the box and click Sign Me Up.
You are now subscribed
Your newsletter sign-up was successful
Want to add more newsletters?

Delivered daily
Kiplinger Today
Profit and prosper with the best of Kiplinger's advice on investing, taxes, retirement, personal finance and much more delivered daily. Smart money moves start here.

Sent five days a week
Kiplinger A Step Ahead
Get practical help to make better financial decisions in your everyday life, from spending to savings on top deals.

Delivered daily
Kiplinger Closing Bell
Get today's biggest financial and investing headlines delivered to your inbox every day the U.S. stock market is open.

Sent twice a week
Kiplinger Adviser Intel
Financial pros across the country share best practices and fresh tactics to preserve and grow your wealth.

Delivered weekly
Kiplinger Tax Tips
Trim your federal and state tax bills with practical tax-planning and tax-cutting strategies.

Sent twice a week
Kiplinger Retirement Tips
Your twice-a-week guide to planning and enjoying a financially secure and richly rewarding retirement

Sent bimonthly.
Kiplinger Adviser Angle
Insights for advisers, wealth managers and other financial professionals.

Sent twice a week
Kiplinger Investing Weekly
Your twice-a-week roundup of promising stocks, funds, companies and industries you should consider, ones you should avoid, and why.

Sent weekly for six weeks
Kiplinger Invest for Retirement
Your step-by-step six-part series on how to invest for retirement, from devising a successful strategy to exactly which investments to choose.
President Trump's administration has made the decision not to cover highly-popular obesity treatments under the 2026 Medicare Advantage and Part D policies. One day after the Senate confirmed Dr. Mehmet Oz as head of the Centers for Medicare and Medicaid Services, the CMS said in a filing that it would not start covering anti-obesity drugs for its beneficiaries.
Legislation passed in 2003 prohibits Medicare, the federal health program for adults 65 and older, from covering medication solely for weight loss. But under President Biden, CMS had proposed reinterpreting the law to allow for the coverage of weight loss drugs for obese, rather than overweight patients. CMS has now decided not to move forward with that coverage.
In an email, Catherine Howden, the spokesperson for CMS said, as reported by CBS, "CMS may consider future policy options for AOMs pending further review of both the potential benefits of these drugs, including updated clinical indications, and relevant costs including fiscal impacts on stakeholders such as state Medicaid agencies."
From just $107.88 $24.99 for Kiplinger Personal Finance
Become a smarter, better informed investor. Subscribe from just $107.88 $24.99, plus get up to 4 Special Issues

Sign up for Kiplinger’s Free Newsletters
Profit and prosper with the best of expert advice on investing, taxes, retirement, personal finance and more - straight to your e-mail.
Profit and prosper with the best of expert advice - straight to your e-mail.
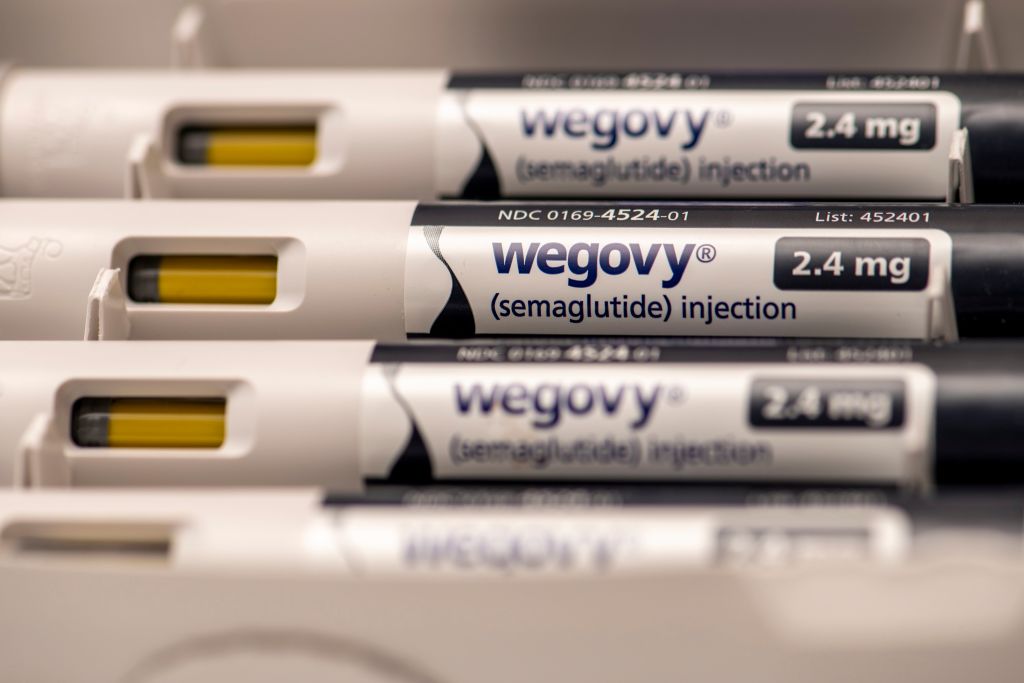
Medicare currently covers drugs that are used for weight loss, like Mounjaro and Ozempic, but only when they are prescribed by doctors for other reasons like managing diabetes. Drugs like Novo Nordisk's Wegovy and Eli Lilly's Zepbound are GLP-1 receptor agonists and were originally developed to treat Type 2 diabetes and certain heart conditions, but have proven highly effective for treating obesity — a chronic condition affecting more than 40% of U.S. adults.
Medicare currently excludes prescriptions only for obesity. While Medicaid programs in all states include GLP-1s prescribed for Type 2 diabetes and certain heart conditions, only 36 states cover at least one of the FDA-approved GLP-1s for obesity (Zepbound, Wegovy, or Saxenda).
The Biden administration proposal on obesity drugs
In November 2024, The Biden administration proposed a rule that would allow both Medicare and Medicaid to cover weight loss drugs beginning in 2026. This rule would expand access to almost 4 million Medicaid users and 3.4 million Medicare users. These drugs can carry a list price of more than $1000 per month, which can be an enormous burden for Americans struggling to afford the blockbuster class of weight loss medications.
Given that the medical community now considers obesity to be a disease, the Biden administration had said, treatment of that disease should be covered by Medicare's Part D prescription drug benefit. The Biden rule was not expected to be finalized until Trump took office.
Who would have qualified for obesity drugs
Older and low-income Americans with a body mass index (BMI) of 30 or higher would have qualified under the Biden rule at the anticipated cost to taxpayers of $35 billion over the next decade, even after taking into account the expected savings from better health outcomes for beneficiaries. Members of Congress on both sides of the aisle agreed that the coverage could ultimately save billions of dollars spent on treating the chronic ailments associated with obesity.
The Biden administration officials did acknowledge that Medicaid programs would also have adopted billions more in costs to cover the weight loss medications, which would be split between the federal government and states. More than a dozen state Medicaid programs already cover drugs for obesity.
What is BMI?
Generally speaking, body mass index or BMI is classified as follows, according to the CDC Trusted Source:
BMI | Meaning |
Less than 18.5 | Underweight |
Between 18.5–24.9 | Average weight |
Between 25-29.9 | Overweight |
Greater than 30 | Obesity |
What does this mean for you?
Under the CMS rule finalized Friday for Medicare plans, the expansion of coverage for weight-loss drugs was not included. This decision means that millions of Americans who rely on Medicare and Medicaid will not have access to coverage for weight loss drugs unless prescribed for other medical reasons. That could limit their treatment options for obesity and lead to higher out-of-pocket costs for those needing these medications.
Despite the stigma around obesity, it can be caused by many things beyond what and how much you eat or exercise. Genetics, certain medications, health conditions and social or economic factors can also play a role. And although living with obesity does not necessarily indicate that you will experience adverse health events, it can increase your risk of several chronic conditions like Type 2 diabetes, heart disease and cancer. It can also reduce your overall quality of life.
The Trump administration has previously said that managing America’s obesity rate is a focus of its ‘Make America Healthy Again’ movement. However, the Secretary of the U.S. Department of Health and Human Services, Robert F. Kennedy Jr., has been skeptical of these injectable weight-loss drugs that have exploded in popularity due to the weight loss some patients have experienced, and has said he wants Americans to focus on their diets rather than relying on medication. Yet, polls show Americans favor having Medicare and Medicaid cover the costs of weight loss drugs.
A 2024 study published in Nature Nutrition & Diabetes estimates the economic costs associated with obesity on major U.S. industries was more than $347 billion in 2023.
Related Content
Profit and prosper with the best of Kiplinger's advice on investing, taxes, retirement, personal finance and much more. Delivered daily. Enter your email in the box and click Sign Me Up.

For the past 18+ years, Kathryn has highlighted the humanity in personal finance by shaping stories that identify the opportunities and obstacles in managing a person's finances. All the same, she’ll jump on other equally important topics if needed. Kathryn graduated with a degree in Journalism and lives in Duluth, Minnesota. She joined Kiplinger in 2023 as a contributor.
-
 Look Out for These Gold Bar Scams as Prices Surge
Look Out for These Gold Bar Scams as Prices SurgeFraudsters impersonating government agents are convincing victims to convert savings into gold — and handing it over in courier scams costing Americans millions.
-
 How to Turn Your 401(k) Into A Real Estate Empire
How to Turn Your 401(k) Into A Real Estate EmpireTapping your 401(k) to purchase investment properties is risky, but it could deliver valuable rental income in your golden years.
-
 My First $1 Million: Retired Nuclear Plant Supervisor, 68
My First $1 Million: Retired Nuclear Plant Supervisor, 68Ever wonder how someone who's made a million dollars or more did it? Kiplinger's My First $1 Million series uncovers the answers.