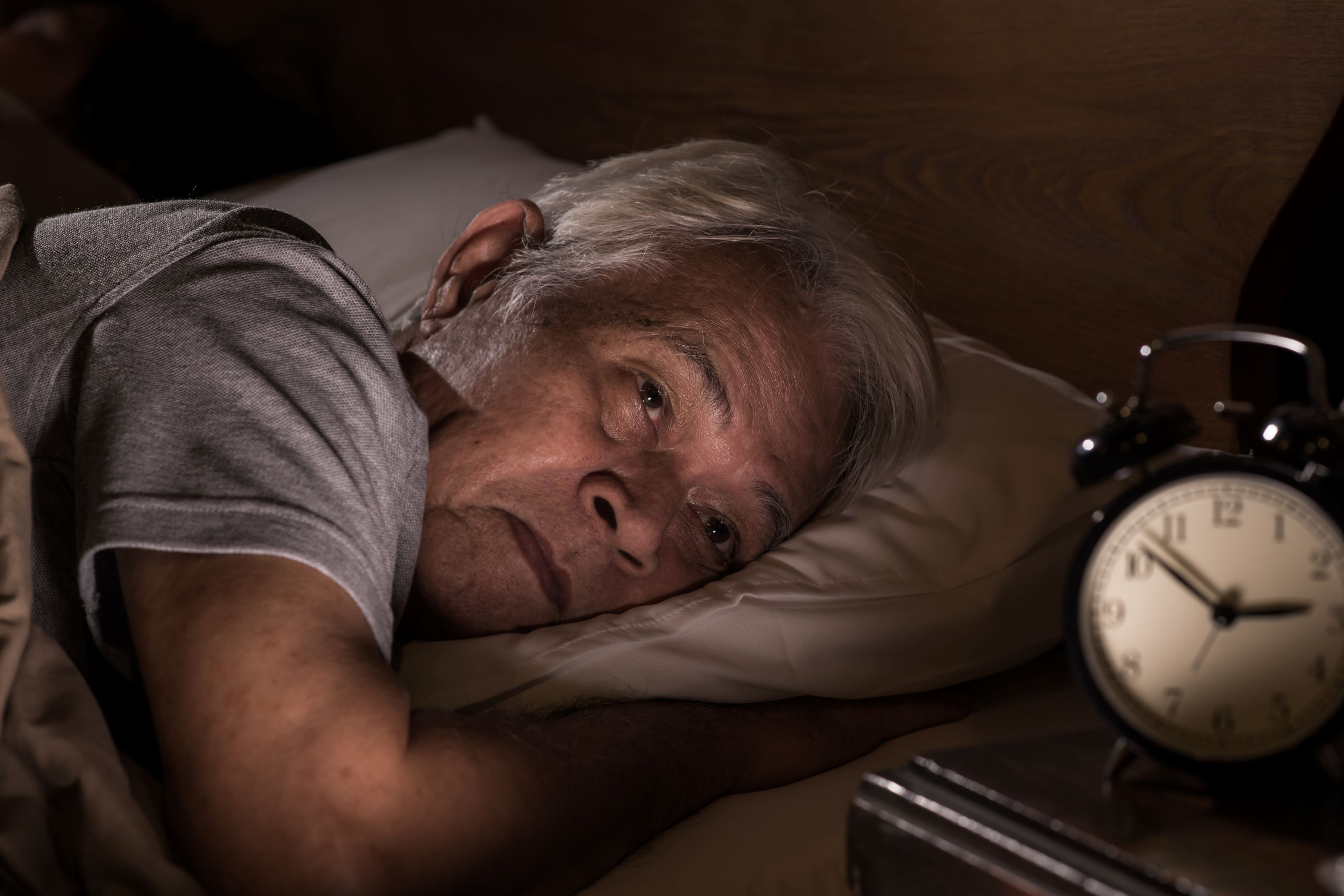
Can't Sleep at Night? Consider Getting Checked Out By a Doctor
Older adults are more likely to suffer from sleep disorders, such as insomnia and sleep apnea. Left untreated these conditions can have dire consequences.
Profit and prosper with the best of Kiplinger's advice on investing, taxes, retirement, personal finance and much more. Delivered daily. Enter your email in the box and click Sign Me Up.
You are now subscribed
Your newsletter sign-up was successful
Want to add more newsletters?

Delivered daily
Kiplinger Today
Profit and prosper with the best of Kiplinger's advice on investing, taxes, retirement, personal finance and much more delivered daily. Smart money moves start here.

Sent five days a week
Kiplinger A Step Ahead
Get practical help to make better financial decisions in your everyday life, from spending to savings on top deals.

Delivered daily
Kiplinger Closing Bell
Get today's biggest financial and investing headlines delivered to your inbox every day the U.S. stock market is open.

Sent twice a week
Kiplinger Adviser Intel
Financial pros across the country share best practices and fresh tactics to preserve and grow your wealth.

Delivered weekly
Kiplinger Tax Tips
Trim your federal and state tax bills with practical tax-planning and tax-cutting strategies.

Sent twice a week
Kiplinger Retirement Tips
Your twice-a-week guide to planning and enjoying a financially secure and richly rewarding retirement

Sent bimonthly.
Kiplinger Adviser Angle
Insights for advisers, wealth managers and other financial professionals.

Sent twice a week
Kiplinger Investing Weekly
Your twice-a-week roundup of promising stocks, funds, companies and industries you should consider, ones you should avoid, and why.

Sent weekly for six weeks
Kiplinger Invest for Retirement
Your step-by-step six-part series on how to invest for retirement, from devising a successful strategy to exactly which investments to choose.
David Csintyan used to boast that he could wake up, answer the telephone on the first ring no matter the time of night and have a lucid conversation. He would also fall asleep before reaching the second page when he reclined on the sofa to read.
But Csintyan, 74, of Monument, Colo., learned that these were warning signs of complex severe sleep apnea after he had an ischemic stroke in 2017. The attending neurologist ordered a sleep study, which uncovered his condition. Up to 70% of stroke patients suffer from sleep apnea. ���I obviously wasn’t getting the quality of sleep I needed, and my brain was not happy by not receiving the oxygen it required,” Csintyan says.
Up to 70 million Americans suffer from a sleep disorder, according to the Centers for Disease Control and Prevention. But older adults have insomnia, sleep apnea and other disorders at higher rates, contributing to other health problems. “The first thing to know about sleep and aging is that the need for sleep doesn’t change as we get older. That’s a myth,” says Sonia Ancoli-Israel, an emeritus professor of psychiatry with a certification in sleep medicine at the University of California-San Diego. “What is true is the ability to get the sleep we need changes. It becomes harder to get that seven to eight hours of sleep, which is recommended for adults.”
From just $107.88 $24.99 for Kiplinger Personal Finance
Become a smarter, better informed investor. Subscribe from just $107.88 $24.99, plus get up to 4 Special Issues

Sign up for Kiplinger’s Free Newsletters
Profit and prosper with the best of expert advice on investing, taxes, retirement, personal finance and more - straight to your e-mail.
Profit and prosper with the best of expert advice - straight to your e-mail.
Aging and Sleep
There are many reasons adults have more trouble sleeping as they age. For one, as you get older, the part of the brain that controls circadian rhythms, which help regulate the sleep-wake cycle, starts to decline, says Dr. Raj Dasgupta, an associate professor of clinical medicine at the Keck School of Medicine at the University of Southern California. In addition, studies show that older adults tend to get less sunlight during the day, exacerbating the issue, Dasgupta says. All of this means the quality and quantity of sleep is affected. “Sleep becomes very fragmented as you get older,” he says. “You will have more awakenings throughout the night so it’s harder to get more restorative sleep.”
Older adults also tend to be prescribed more medications, which can interfere with sleep, Ancoli-Israel says. If a person is experiencing pain related to another condition, such as arthritis or cancer, that can also prevent sleep, she adds.
Common Types of Sleep Disorders
Overall, there are about 60 to 70 sleep disorders, according to Dr. Charu Sabharwal, who is board certified in sleep medicine and owner of Comprehensive Sleep Care Center, which has nine locations in Maryland and Virginia. The most common disorder for older adults is trouble falling or staying asleep, otherwise known as insomnia. Stress, lack of exercise, poor sleep habits, medications or pain from another condition are all causes. Insomnia is considered chronic if you have issues three nights a week for at least three months.
Sleep apnea is another common condition. It occurs when a person repeatedly stops breathing while asleep. This can be caused by the brain failing to give the right signals to keep you breathing, a condition called central sleep apnea. Obstructive sleep apnea is caused by excess tissue in the back of the throat or the muscles there becoming too relaxed, which blocks the airway, making it difficult to breathe.
About 18% of men between the ages of 61 and 100 suffer from sleep apnea, according to the American Thoracic Society, a nonprofit that supports improving care for critical illnesses, sleep-related breathing disorders and pulmonary diseases. Women who have gone through menopause tend to have sleep apnea at about the same rate as men, Sabharwal says.
Not getting treatment for a sleep disorder can have dire consequences. Theresa Shumard, community and education manager at the American Sleep Apnea Association, notes that leaving sleep apnea untreated can affect your personality. “When someone is so sleep deprived because hundreds of times a night they are not breathing, they can become a person who isn’t engaged in family activities,” she says. “Their personalities might be grouchy.”
Insomnia and insufficient sleep are linked to increased risk of accidents, slower reaction times and problems with attention, memory and concentration, Ancoli-Israel says. Adults who get less than seven hours of sleep per day are more likely to suffer from 10 other chronic health conditions, including coronary heart disease and stroke, according to the CDC.
Csintyan believes that his sleep apnea caused his stroke, though his doctors never explicitly said so. He says his primary care physician was shocked to hear he had a stroke given his excellent health and lack of risk factors. “I’m convinced that that trip to the hospital would have been unnecessary,” says Csintyan, who is a peer mentor in the American Sleep Apnea Association AWAKE (which stands for “alert, well and keeping energetic”) Program. He educates people about the disorder and its treatment.
Getting Treatment for a Sleep Disorder
You should seek treatment for a potential sleep disorder if you’ve had difficulty falling or staying asleep for two to four weeks after trying simple fixes, such as cutting out screen time before bed and maintaining a regular schedule, Sabharwal says. The American Sleep Association has tips for getting a good night sleep on its website in the “About Sleep” section. “If it’s not treated in a timely manner, it could become a pattern and then we call that chronic insomnia,” she says. “The sooner we pull the patient out of the pattern, the better.”
Waking up extremely early or feeling unrested are other signs of a potential problem. If your bed partner notices that you snore or stop breathing at night, you should get checked out.
Insurance, including Medicare, should cover visiting a specialist, usually a neurologist, pulmonologist or internist with additional training in sleep medicine. Insomnia is diagnosed based on your medical history and is usually treated with cognitive behavioral therapy to undo any bad habits that interfere with sleep, such as watching television in bed. Insomniacs are also taught relaxation techniques and breathing exercises.
Many people automatically think of sleeping pills for treatment, but medication should be a last resort as most of these pills are not approved for patients to use for more than six months because they are habit forming, Sabharwal says. A doctor can review a patient’s medications for other conditions and make adjustments. For example, a pill that causes drowsiness can be taken in the evening rather than the morning, Ancoli-Israel says.
A sleep study, which insurance should cover, may be required to diagnose sleep apnea and other disorders. You may need to spend the night at a clinic where your sleep stages, breathing, oxygen levels in your blood and eye movements are measured. At-home sleep studies have become more popular during the pandemic but can only be used to diagnose sleep apnea and may be inaccurate if the patient uses the equipment incorrectly, Sabharwal says.
Treatments vary depending on the severity of sleep apnea. For mild or moderate cases, a dental device, which is created by a dentist and then adjusted by a sleep physician, prevents the tongue from falling back and closing off the patient’s airway, Sabharwal says. Another treatment involves inserting a battery about the size of a quarter under the patient’s skin that connects to a nerve and keeps the tongue from interfering with breathing during sleep. The battery can be turned on and off by touching the skin with a small remote.
More severe cases may require the person to wear a continuous positive airway pressure, or CPAP, machine, which uses air pressure to keep the airway open. More than 100 types of masks can be used with these machines, and a trained technician can offer multiple options to find the right one for you. Your insurance should pay for a new mask every 90 days.
Up to half of patients stop using their CPAP machine in the first year because the equipment is uncomfortable, but sticking with a treatment for a sleep disorder is vital, given its link to more serious conditions. Several years before Csintyan’s stroke, he underwent a sleep study and was diagnosed with nighttime oxygen desaturation, which is a lower concentration of oxygen in the blood while someone is asleep. He was supposed to use a device to help provide him with oxygen, but the equipment was cumbersome. He also didn’t fully understand how serious the diagnosis was so he stopped using the machine after about six months, a decision he now regrets.
He encourages others to ask their doctors to clearly explain any diagnosis and its potential link to other conditions. “It may be life’s single best blessing to help you avoid or mitigate other diseases,” he says.
Profit and prosper with the best of Kiplinger's advice on investing, taxes, retirement, personal finance and much more. Delivered daily. Enter your email in the box and click Sign Me Up.
Jackie Stewart is the senior retirement editor for Kiplinger.com and the senior editor for Kiplinger's Retirement Report.
-
 Dow Leads in Mixed Session on Amgen Earnings: Stock Market Today
Dow Leads in Mixed Session on Amgen Earnings: Stock Market TodayThe rest of Wall Street struggled as Advanced Micro Devices earnings caused a chip-stock sell-off.
-
 How to Watch the 2026 Winter Olympics Without Overpaying
How to Watch the 2026 Winter Olympics Without OverpayingHere’s how to stream the 2026 Winter Olympics live, including low-cost viewing options, Peacock access and ways to catch your favorite athletes and events from anywhere.
-
 Here’s How to Stream the Super Bowl for Less
Here’s How to Stream the Super Bowl for LessWe'll show you the least expensive ways to stream football's biggest event.
-
 9 Types of Insurance You Probably Don't Need
9 Types of Insurance You Probably Don't NeedFinancial Planning If you're paying for these types of insurance, you may be wasting your money. Here's what you need to know.
-
 Amazon Resale: Where Amazon Prime Returns Become Your Online Bargains
Amazon Resale: Where Amazon Prime Returns Become Your Online BargainsFeature Amazon Resale products may have some imperfections, but that often leads to wildly discounted prices.
-
 457 Plan Contribution Limits for 2026
457 Plan Contribution Limits for 2026Retirement plans There are higher 457 plan contribution limits in 2026. That's good news for state and local government employees.
-
 Medicare Basics: 12 Things You Need to Know
Medicare Basics: 12 Things You Need to KnowMedicare There's Medicare Part A, Part B, Part D, Medigap plans, Medicare Advantage plans and so on. We sort out the confusion about signing up for Medicare — and much more.
-
 The Seven Worst Assets to Leave Your Kids or Grandkids
The Seven Worst Assets to Leave Your Kids or Grandkidsinheritance Leaving these assets to your loved ones may be more trouble than it’s worth. Here's how to avoid adding to their grief after you're gone.
-
 SEP IRA Contribution Limits for 2026
SEP IRA Contribution Limits for 2026SEP IRA A good option for small business owners, SEP IRAs allow individual annual contributions of as much as $70,000 in 2025, and up to $72,000 in 2026.
-
 Roth IRA Contribution Limits for 2026
Roth IRA Contribution Limits for 2026Roth IRAs Roth IRAs allow you to save for retirement with after-tax dollars while you're working, and then withdraw those contributions and earnings tax-free when you retire. Here's a look at 2026 limits and income-based phaseouts.
-
 SIMPLE IRA Contribution Limits for 2026
SIMPLE IRA Contribution Limits for 2026simple IRA For 2026, the SIMPLE IRA contribution limit rises to $17,000, with a $4,000 catch-up for those 50 and over, totaling $21,000.